Introduction to TMJ Disorders
As a dentist, you are often the first healthcare professional to recognize the signs of temporomandibular joint (TMJ) disorders, also known as temporomandibular dysfunction (TMD). These disorders involve the complex musculoskeletal system of the jaw and can have a significant impact on your patients’ oral health, comfort, and overall quality of life.
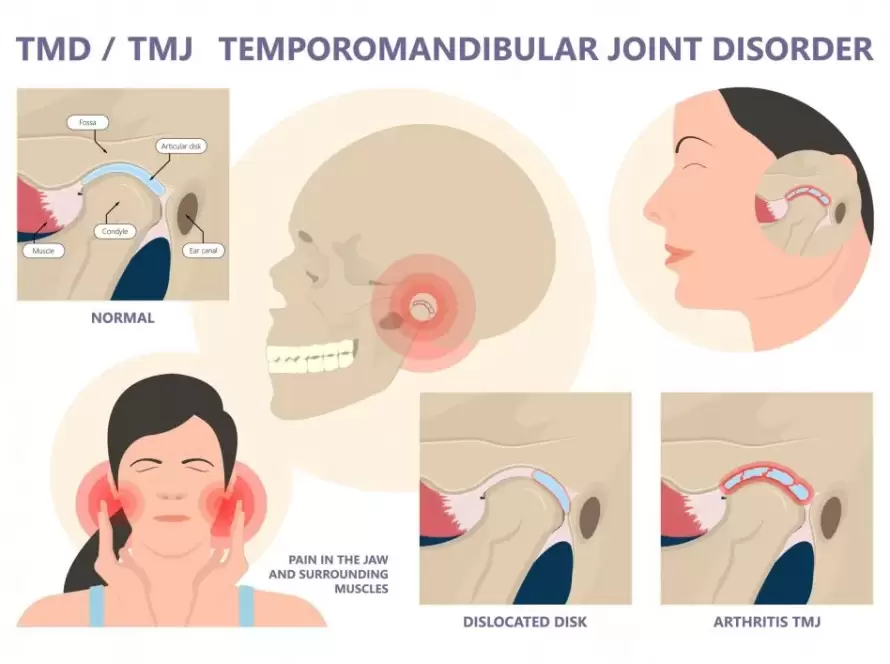
The temporomandibular joint (TMJ) connects the lower jaw (mandible) to the skull (temporal bone) and allows for essential jaw movements like chewing, speaking, and swallowing. Symptoms in TMD include jaw joint discomfort such as jaw clicking, locking, pain in Jaw, ear pain, ear stuffiness, headaches, and poor sleep. As a dentist, understanding the causes, symptoms, and treatment options for TMJ disorders is critical for effectively diagnosing and managing these conditions in your patients.
The exact cause of TMD is unknown
TMJ disorders can arise from a variety of factors, and in many cases, they are multifactorial. As a dentist, it’s important to consider the following potential causes:
- Bruxism: Chronic teeth grinding and jaw clenching, often exacerbated by stress, can cause wear on the teeth and place excessive pressure on the TMJ, leading to pain and inflammation.
- Trauma: Injury to the jaw, head, or neck (e.g., whiplash or a direct blow to the face) can result in TMJ dysfunction, especially if the joint is displaced or damaged.
- Arthritis: Degenerative conditions like osteoarthritis or rheumatoid arthritis can affect the TMJ, leading to joint degeneration, inflammation, and limited movement.
- Headache disorders: TMJ pain may be due to headache disorders such as migraines or other types.
- Systemic Illnesses: Immunological, neurological, sleep disorders, and other medial conditions may play a role in mechanism of TMD.
Key Symptoms of TMJ Disorders
When a patient presents with potential TMJ disorders, it’s essential to assess their symptoms thoroughly. Common signs of TMD include:
- Jaw Pain and Tenderness: This is the most common symptom and can be localized to the TMJ or radiate to the face, neck, or shoulders.
- Clicking, Popping, or Grinding Noises: Audible sounds when opening or closing the mouth, often accompanied by pain, may indicate joint dysfunction.
- Limited Jaw Movement: Patients may report difficulty opening their mouth fully, or they may experience a sensation of the jaw “locking” or “catching.”
- Headaches: Tension and dysfunction in the TMJ can trigger frequent headaches, often resembling tension-type or migraine headaches.
- Ear-related Symptoms: Tinnitus (ringing in the ears), earaches, or a feeling of fullness in the ears may be related to TMJ disorders.
- Facial Pain: Patients might complain of dull or sharp pain in the face, especially around the temples or jaw.
- Neck and Shoulder Pain: Muscular tension in the neck and shoulders is frequently seen in patients with TMD, especially those with bruxism or clenching habits.
Diagnosing TMJ Disorders
Accurate diagnosis of TMJ disorders requires a comprehensive approach. Here’s how dentists can assess and diagnose TMD:
- Patient History: Start by taking a thorough history to identify risk factors such as bruxism, trauma, or chronic stress. Ask about any associated symptoms like headaches, ear pain, or facial discomfort.
- Physical Examination: Palpate the TMJ while the patient opens and closes their mouth. Look for signs of swelling, clicking, or tenderness in the joint and surrounding muscles.
- Range of Motion: Evaluate the patient’s ability to open and close their mouth fully. Any limitation or deviation in movement can indicate TMJ dysfunction. Jaw opening of about 3 fingers wide is usually adequate.
- Occlusion Examination: Assess the patient’s bite and look for signs of malocclusion, tooth wear, or signs of bruxism (e.g., worn or fractured teeth).
- Imaging: In some cases, advanced imaging like MRI or CBCT (Cone Beam CT) scans may be required to evaluate soft tissue changes or joint damage.
Treatment Options for TMJ Disorders
While many TMJ disorders are self-limiting, treatment is often necessary to alleviate symptoms and prevent further damage. Dentists can offer a variety of treatments, depending on the severity of the condition:
- Occlusal Splints and Night Guards: These devices help to reduce the effects of bruxism and teeth grinding by redistributing bite forces and protecting the TMJ. Custom-made occlusal splints are often the first line of treatment for mild to moderate TMJ dysfunction.
- Physical Therapy: Encourage patients to engage in jaw exercises to improve joint mobility, strengthen muscles, and reduce pain. A trained physical therapist specializing in TMJ can provide targeted exercises.
- Behavioral Therapy: Stress management, relaxation techniques, and counseling may help patients reduce clenching and grinding habits, which can exacerbate TMD.
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants may be prescribed to reduce pain and inflammation. In some cases, corticosteroid injections or botulinum toxin (Botox) injections are used to alleviate muscle spasms.
- Surgical Intervention: In rare, severe cases where conservative treatments fail, surgical procedures like arthroscopy or open joint surgery may be considered. However, surgery should always be a last resort.
How TMJ Disorders Affect Your Patients’ Lives
TMJ disorders can significantly disrupt a patient’s quality of life. The pain and discomfort associated with TMD can affect multiple aspects of daily living, including:
- Eating and Drinking: Chewing may become painful or difficult, which can affect diet and nutrition.
- Sleep: Pain, jaw clenching, or bruxism can interfere with sleep quality, leading to fatigue and irritability.
- Work and Social Life: Chronic pain and discomfort can make it harder for patients to engage in their regular work and social activities.
- Emotional and Mental Health: Ongoing pain and discomfort can lead to frustration, anxiety, and depression, as patients struggle with both physical and emotional stress.
Conclusion
TMJ disorders are complex conditions that can have a major impact on your patients’ well-being. As a dentist, you play a crucial role in identifying, diagnosing, and managing TMD. Early intervention can help prevent long-term damage to the temporomandibular joint and improve your patients’ quality of life. By understanding the causes, symptoms, and treatment options, you can provide comprehensive care and help your patients find relief from this often misunderstood condition.