As a dentist, you are often the first healthcare provider to identify symptoms of temporomandibular joint (TMJ) disorders, which affect millions of people worldwide. TMJ dysfunction can cause a range of symptoms, including jaw pain, clicking or popping sounds, headaches, and even difficulty chewing. While many cases can be managed through dental care, there are instances where a TMJ specialist—such as an oral surgeon, physical therapist, or pain management expert—may be needed for advanced evaluation and treatment.
Knowing when to refer a patient to a TMJ specialist is key to ensuring they receive the appropriate care and avoid long-term complications. In this blog, we will outline the **guidelines for when to refer a patient to a TMJ specialist**, and how doing so can lead to more effective, targeted treatment.
1. Persistent or Severe Pain
One of the most common reasons patients seek dental care for TMJ disorders is jaw pain. If a patient has been experiencing chronic jaw pain that doesn’t respond to basic treatments like over-the-counter pain relievers or custom splints, it may be time to refer them to a specialist.
Signs that pain may require specialist attention:
– Persistent jaw pain that lasts for more than a few weeks or recurs frequently.
– Severe pain that interferes with daily activities, such as speaking, eating, or even resting.
– Pain that is not alleviated by conservative treatments, such as heat/cold therapy, or bite splints.
If a patient’s pain is severe or chronic and not improving with typical dental interventions, a TMJ specialist can conduct a more detailed assessment to explore the underlying causes of the pain, such as joint degeneration or structural issues, and recommend specialized treatment options like injections, physical therapy, or surgery.
2. Difficulty Moving the Jaw
A limited range of motion or difficulty moving the jaw is another reason to consider referring a patient to a TMJ specialist. If the jaw locks or the patient is unable to open their mouth wide enough to eat or speak, this could indicate more severe TMJ dysfunction or even joint displacement.
Signs of restricted jaw movement:
– Difficulty opening the mouth (less than 35 mm of mouth opening).
– Jaw locking or catching, where the jaw becomes stuck in a closed or open position.
– Severe discomfort during jaw movement, especially while chewing or speaking.
In these cases, a TMJ specialist can determine whether there is structural damage to the joint, such as disc displacement or degeneration, and recommend appropriate interventions like joint manipulation, an occlusal orthotic (a bit more complex then a simple bite guard), trigger point injections, nerve blocks, ganglion blocks, Chemogenervation (botox), steriod injections, sodium hyaluronate injections, joint manipulation, acupuncture (DR. Chandwani is trained in acupuncture).
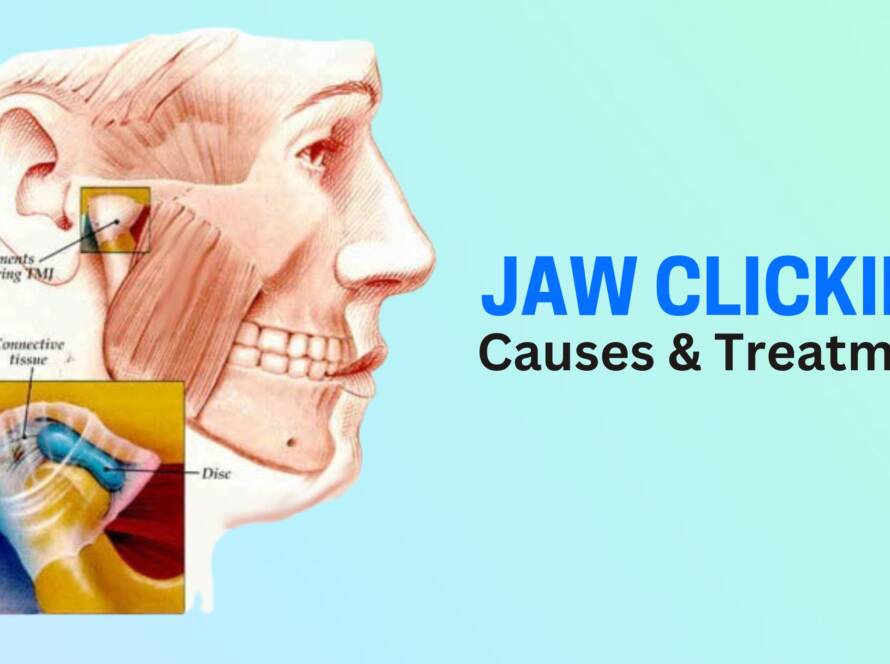
3. Clicking, Popping, or Grinding Sounds
Occasional clicking or popping sounds in the jaw may not necessarily be a cause for concern. However, if these sounds are persistent, painful, or associated with limited jaw movement or discomfort, it could signal a deeper issue with the temporomandibular joint or surrounding muscles.
When clicking or popping warrants a referral:
– Frequent or painful clicking/popping sounds when opening or closing the mouth.
– Grinding or grating sounds that are loud and associated with jaw pain or muscle fatigue.
– Inability to move the jaw smoothly, which may indicate internal joint damage.
A TMJ specialist can evaluate the source of these sounds and determine whether there is damage to the joint’s cartilage, bone, or surrounding muscles. Treatment options might include physical therapy, oral appliances, joint injections, or in some cases, arthrocentesis (a minimally invasive procedure to flush out the joint) or arthroscopy.
4. Headaches and Migraines Linked to TMJ
Many patients with TMJ disorders suffer from headaches or migraines as a secondary symptom. These headaches are often caused by the tension in the jaw and surrounding muscles, but they can also be a sign of deeper TMJ dysfunction. If the patient is experiencing chronic headaches that seem related to their jaw symptoms and are not responding to typical headache treatments, a referral to a TMJ specialist is warranted. Some headaches get triggered by TMJ disorders also.
Signs that headaches require specialist care:
– Frequent tension headaches or migraines that correlate with jaw discomfort or clicking sounds.
– Headaches that do not respond to over-the-counter pain medications or treatments. Morning headaches are very commonly related to night time jaw tensing.
– Jaw pain that triggers or worsens headaches.
A TMJ specialist can help address the headaches by evaluating jaw and offering specialized treatments like muscle relaxation therapy, or even botulinum toxin (Botox) injections to relieve muscle tension in severe cases.
5. Signs of Bruxism (Teeth Grinding)
Bruxism—involuntary grinding or clenching of the teeth, often during sleep—is a common issue for people with TMJ disorders. If a patient is grinding their teeth to the point of tooth damage, worn-down teeth, or severe muscle pain, it may be necessary to refer them to a TMJ specialist for a more targeted treatment plan.
Signs of bruxism requiring referral:
– Severe tooth wear, chipping, or fractures.
– Painful or tight jaw muscles due to clenching.
– Persistent headaches or earaches related to grinding.
A TMJ specialist can provide additional treatments like biofeedback, physical therapy, or medications to manage bruxism. If needed, they may suggest more advanced therapies like botulinum toxin (Botox) injections or splints designed to reduce clenching or grinding during sleep.
6. Possible Structural Issues in the TMJ
If a patient’s symptoms suggest that there may be **structural damage** to the TMJ, such as joint displacement, disc derangement, or other anatomical issues, a referral to a TMJ specialist is essential for a thorough examination. Imaging, such as an MRI or CT scan, may be necessary to diagnose the extent of the damage.
Signs of structural TMJ problems:
– Jaw locking*(unable to open or close the mouth).
– Discomfort or pain that seems to originate from the joint itself (deep inside the ear or jaw).
– A history of trauma or injury to the jaw (e.g., whiplash or sports injuries).
TMJ specialists can recommend advanced imaging techniques to assess the joint’s structure and offer interventions such as arthrocentesis, joint injections, or surgical repair to address severe cases.
7. When Conservative Treatments Are Ineffective
Many TMJ disorders can be managed conservatively with simple interventions like custom splints, physical therapy, and stress management techniques. However, if a patient’s symptoms persist despite these efforts, it may be time to refer them for more advanced care.
Indications for referral when conservative treatments fail:
– Continued pain or discomfort despite the use of bite splints or mouthguards.
– Limited jaw movement that doesn’t improve with physical therapy.
– Excessive muscle tenderness or jaw dysfunction that remains unaddressed after dental care.
A TMJ specialist can explore more advanced treatments, such as injections, surgical options, or advanced physical therapy techniques tailored to the patient’s specific needs.
8. Conclusion: The Importance of Early Referral
TMJ disorders can cause significant discomfort and negatively impact a patient’s quality of life, especially if left untreated. As a dentist, recognizing when to refer a patient to a TMJ specialist is crucial in ensuring that they receive the most appropriate care. If you notice that a patient’s symptoms are severe, persistent, or unresponsive to standard treatments, a referral to a TMJ specialist can help identify underlying causes and provide more effective, targeted interventions.